Liver Cirrhosis: Causes, Symptoms, and Treatment Options
What Is Liver Cirrhosis?
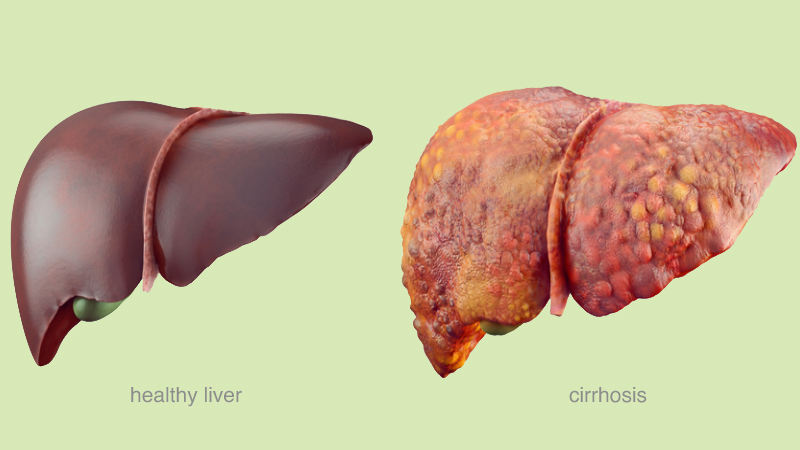
Liver cirrhosis is a chronic and progressive condition characterized by gradually replacing healthy liver tissue with scar tissue. This scarring affects the normal structure and function of the liver, leading to impaired liver function over time.
The liver is a vital organ responsible for various functions, including detoxification of harmful substances, production of proteins, metabolism of nutrients, and storage of vitamins and minerals. When cirrhosis occurs, the liver becomes hardened and nodular due to the formation of fibrous scar tissue.
What Are The Symptoms Of Liver Cirrhosis?
Liver cirrhosis can present a wide range of symptoms, and the severity and progression of symptoms can vary among individuals. Some common symptoms of liver cirrhosis include:
- Fatigue and weakness
- Jaundice
- Loss of appetite and weight loss
- Abdominal swelling and pain
- Nausea and vomiting
- Easy bruising and bleeding
- Mental confusion and changes in cognition
- Spider-like blood vessels (spider angiomas) may appear on the skin, especially the upper body.
If you suspect, you may have liver cirrhosis or are experiencing any concerning symptoms. It is crucial to seek medical attention for proper evaluation and diagnosis.
What Are the Causes of Liver Cirrhosis?
Liver cirrhosis can be caused by various factors that lead to chronic liver damage and the subsequent development of scar tissue. Here are some common causes of liver cirrhosis:
- Excessive and prolonged alcohol consumption is a leading cause of liver cirrhosis.
- Chronic infection with hepatitis B virus (HBV) or hepatitis C virus (HCV) can cause ongoing inflammation in the liver, leading to cirrhosis if left untreated.
- Non-alcoholic Fatty Liver Disease (NAFLD) and Non-alcoholic Steatohepatitis (NASH)
- Autoimmune Hepatitis occurs when the immune system attacks the liver, resulting in inflammation and damage to the liver.
- Primary Biliary Cholangitis (PBC) is a chronic autoimmune disease that primarily affects the small bile ducts within the liver. These ducts become inflamed, leading to liver damage and, eventually, cirrhosis.
- Hemochromatosis is a hereditary condition characterized by excessive absorption and accumulation of iron in the body, including the liver.
- Wilson's Disease:This rare inherited disorder impairs the liver's ability to metabolize copper, leading to its accumulation in the liver and other organs.
- Prolonged exposure to certain medications, industrial toxins, and environmental pollutants can cause liver damage and, in some cases, cirrhosis. Examples include long-term use of high-dose acetaminophen (paracetamol), methotrexate, and excessive exposure to aflatoxins.
- Certain rare genetic disorders, such as alpha-1 antitrypsin deficiency, glycogen storage diseases, and cystic fibrosis, can also lead to liver cirrhosis.
How Can Liver Cirrhosis Be Prevented?
While not all causes of liver cirrhosis are preventable, there are several steps individuals can take to reduce the risk of developing the condition or slow down its progression:
- Limit Alcohol Consumption.
- Prevent Viral Hepatitis Infections. Hepatitis B and C infections are the leading causes of liver cirrhosis. It is important to practice safe sex, avoid sharing needles or other drug paraphernalia, and take precautions to prevent exposure to infected blood.
- Maintain a Healthy Weight and Diet. Adopting a healthy lifestyle that includes regular exercise and a balanced diet can help manage weight and prevent or manage NAFLD.
- Practice Safe Medication Use: Some medications, such as acetaminophen (paracetamol), can cause liver damage if taken excessively or over a long period. Follow the recommended dosage and duration of use for medications, and consult a healthcare professional if you have any concerns or questions.
- Minimize exposure to toxins and chemicals that can damage the liver. This includes avoiding contact with industrial chemicals, using protective measures when handling toxic substances, and following safety guidelines in the workplace.
How Is Liver Cirrhosis Diagnosed?
Liver cirrhosis is diagnosed through a comprehensive evaluation that includes various diagnostic tools and tests. The following methods are commonly used in the diagnosis of liver cirrhosis:
- Medical history assessment: Your healthcare provider will inquire about your symptoms, medical history, alcohol consumption, and exposure to risk factors.
- Physical examination: A thorough physical examination will be conducted to check for signs of liver disease, such as jaundice, abdominal swelling, and spider angiomas.
- Blood tests: These tests assess liver function, including liver enzyme levels, liver function panel, bilirubin levels, clotting factors, and viral hepatitis markers.
- Imaging studies: Ultrasound, CT scan, and MRI are used to visualize the liver, evaluate its structure, detect abnormalities, and assess blood flow.
- FibroScan: This non-invasive test measures liver stiffness as an indicator of fibrosis and cirrhosis.
- Liver biopsy: In some cases, a liver biopsy may be performed to confirm the diagnosis and assess the extent of liver damage.
By combining these diagnostic approaches, healthcare professionals can determine the presence and severity of liver cirrhosis, identify the underlying cause, and plan appropriate treatment and management strategies.
Treatment Options for Liver Cirrhosis:
Liver cirrhosis treatment aims to manage complications, slow disease progression, and enhance the quality of life. The specific approach depends on the underlying cause and individual health. Here are common treatment options
Lifestyle Modifications:
- Alcohol cessation: Crucial for alcohol-related cirrhosis.
- Healthy diet: Balanced with reduced salt intake to manage fluid retention and support liver health.
- Weight management: Regular exercise and proper nutrition to maintain a healthy weight, especially for non-alcoholic fatty liver disease (NAFLD).
Medications:
- Manage complications: Prescribed medications, like diuretics for fluid retention or beta-blockers for portal hypertension.
- Antiviral therapy: Suppresses viral replication and reduces liver inflammation in viral hepatitis-related cirrhosis.
Liver Transplantation:
For severe cases, replacing the diseased liver with a healthy one from a deceased or living donor.
Symptom Management:
- Medications: Alleviate fatigue, itching, and pain associated with cirrhosis.
- Nutritional support: Recommended supplements to ensure proper nutrient intake.
Ongoing Monitoring and Follow-up:
- Regular check-ups and liver function monitoring to assess disease progression, manage complications, and adjust treatment as needed.
Remember, treatment plans should be personalized and guided by healthcare professionals specialized in liver diseases. Early detection, managing underlying causes, and proactive treatment can enhance outcomes and quality of life for individuals with liver cirrhosis.


 WhatsApp
WhatsApp